The otitis media is one of the most commonly treated infections.
In acute otitis media (AOM), the disease process is usually limited only to the mucoperiosteal lining of the middle ear cleft, but when it breaks into the bony walls of the cleft like in the case of CHOLESTEATOMA, various complications can arise.
Complications can occur as the result of bony destruction from either hyperemic decalcification in AOM or chronic bioenzymatic activity in cholesteatoma.
In the pre-antibiotic era, AOM frequently led to intratemporal and intracranial complications and therefore had high morbidity.
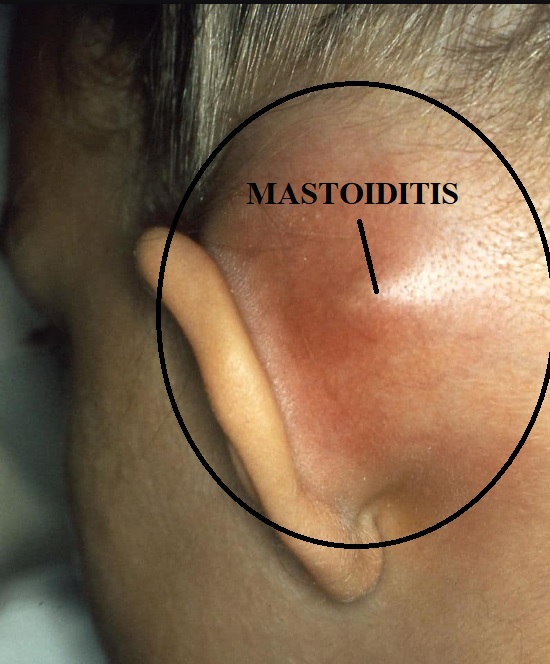
Acute mastoiditis is the inflammation of the mucosal lining of the antrum and mastoid air cells that invariably occurs in AOM. However, in “mastoiditis,” which is now relatively rare, the infection involves bony walls of the mastoid air cells.
Ear pain and tenderness extending into the postauricular region and fever are hallmark /symptoms.

Protrusion of the pinna and postauricular erythema and swelling are classic findings.
Etiology and Predisposing Factors
1. Acute otitis media especially in cases of measles, exanthematous fevers, poor nutrition, and diabetes.
2. Microorganisms: Beta-hemolytic streptococci (most common) and other organisms causing AOM.
Anaerobic organisms are also common.
3. Mastoids with well-developed mastoid air cells.
4. Children are affected more.
Pathology of Acute Mastoiditis –
Acute mastoiditis can manifest in two ways —
1. Acute periostitis (inflammation of periosteum):
The spread of infection occurs via venous channels.
2. Acute osteitis (coalescent mastoiditis):
Destruction of mastoid air cells trabeculae.
The pathological processes include —
a) Production of pus under tension
The inflammatory process to the mucoperiosteal lining increases the amount of pus. the drainage of pus through a small perforation of the tympanic membrane (TM) and the Eustachian tube (ET) cannot keep pace with the amount of pus production. Swollen mucosa of the antrum and attic impede the drainage and result in further accumulation of pus
b) Hyperemic decalcification and osteoclastic resorption of bony walls
Hyperemia causes the dissolution of calcium from the mastoid air cells (hyperemic decalcification).
The destruction and coalescence of mastoid air cells convert mastoid into a single large cavity, which is filled with pus and also called “ EMPYEMA MASTOID ”. The mastoid cortex may be broken leading to a subperiosteal abscess which can burst the overlying skin and result in discharging fistula.
Clinical Features of Acute Mastoiditis –
The change in the character and reappearance of clinical features during the resolving AOM points to the development of acute mastoiditis.
1) Pain behind the ear in the mastoid region.
2) Fever:
Usually low grade. In children, fever is high with a rise in pulse rate.

3) Ear discharge:
Profuse and increases in purulence.
The persistence of otorrhea beyond 3 weeks in a case of AOM indicates mastoiditis.
The discharge may cease (due to obstruction in its drainage) with progressive worsening of clinical features.
Mucopurulent or purulent discharge is often PULSATILE (known as LIGHT-HOUSE EFFECT ). It comes through the perforation of pars tensa.
4) Mastoid tenderness
Tenderness may be present over the middle of the mastoid process, mastoid tip, posterior border, or root of the zygoma.
The Tenderness over the supramental triangle may be seen in AOM due to inflammation of the mastoid antrum. It may be compared with that of the healthy side.
5) Sagging of posterosuperior meatal wall
It indicates periostitis of the bony wall that lies between the antrum and deep bony canal.
6) Perforation of tympanic membrane
A small central perforation or nipple-like protrusion is seen in pars tensa with congestion of the remaining TM.
The TM may remain intact (inadequate antibiotics treatment) but looks dull and opaque.
7) Swelling over the mastoid region
Edema of periosteum imparts a smooth “ironed out” feeling over the mastoid. If pus bursts bony cortex, a subperiosteal fluctuant abscess is seen. The pinna is pushed forward and downwards.
8) Conductive hearing loss.
9) General appearance: Ill and toxic look.
Investigations for Acute Mastoiditis —
1) CBC:
Polymorphonuclear leukocytosis and raised ESR.
2) CT temporal bone
Loss of bony trabeculae indicates coalescent mastoiditis. CT can also identify other intracranial or neck abscesses.
3) Culture and sensitivity of ear discharge
To know the organism and the antibiotics to which they are sensitive.
Differential Diagnoses of Acute Mastoiditis –
1) Suppuration of mastoid lymph nodes:
Scalp infection can lead to postauricular lymphadenopathy, which though rarely suppurates and leads to abscess formation. There is no history of preceding otitis media and TM is normal. The abscess is quite superficial.
2) Furunculosis of the external auditory canal (EAC)
Treatment of Acute Mastoiditis –
The majority of the cases of acute mastoiditis usually respond to culture-directed intravenous antibiotics and myringotomy with or without a tympanostomy tube.
1) Hospitalization and antibiotics:
These patients need intravenous antibiotics in high doses.
Till the report of culture and sensitivity, amoxicillin or ampicillin. As the anaerobic organisms are present, metronidazole is in addition.
2) Myringotomy:
Small TM perforation is insufficient, and wide myringotomy facilitates pus drainage.
3) Cortical mastoidectomy:
The cortical mastoidectomy exenterates all mastoid air cells along with the removal of pockets of pus. Adequate antibiotic treatment: 5–10 days postoperatively.
The indications include the following —
- Subperiosteal abscess.
- Sagging of posterosuperior meatal wall.
- Positive reservoir sign: External auditory canal fills with pus immediately after the cleaning.
- No improvement or worsening of the condition in spite of adequate medical treatment for 48 hours.
- Complications: Facial paralysis, labyrinthitis, and intracranial complications.
Complications of Acute Mastoiditis –
They include —
1) Subperiosteal Abscess,
2) Labyrinthitis,
3) Facial paralysis,
4) Petrositis,
5) Extradural abscess,
6) Subdural abscess,
7) Meningitis,
8) Brain abscess,
9) Lateral sinus thrombophlebitis, and
10) Otitic hydrocephalus.
THANK YOU
MEDICAL ADVICE DISCLAIMER:
This blog including information, content, references, and opinions is for informational purposes only.
The Author does not provide any medical advice on this platform.
Viewing, accessing, or reading this blog does not establish any doctor-patient relationship.
The information provided in this blog does not replace the services and opinions of a qualified medical professional who examines you and then prescribes medicines.
And if you have any questions of medical nature, please refer to your doctor or the qualified medical personnel for evaluation and management at a clinic/hospital near you.
The content provided in this blog represents the Author’s own interpretation of research articles.